Discover How Gough Surgical, PLLC Is Unleashes Advanced Robotic Orthopedic Surgery in Unprecedented Ways – Planet TV Studios Brings You Documentary Series New Frontiers.
Planet TV Studios displays a visual report pertaining to Dr. Brandon Gough's Advances in Surgical Techniques within "New Frontiers" — Premiering the month of March 2024 across Countrywide TV & On-Demand.
BOCA RATON, FL, UNITED STATES, March 1, 2024 /ReportWire.org -- Planet TV Studios humbly introduces its state-of-the-art documentary lineup, "New Frontiers," featuring the cutting-edge triumphs of Gough Surgical, PLLC. This series investigates the major breakthroughs guided by Dr. Brandon Gough, M.D., a top-tier orthopedic surgeon proficient in cutting-edge microinvasive techniques plus robotic surgery for hip and knee replacements.
"New Frontiers" embodies a mesmerizing investigation expertly crafted in order to exhibit visionary organizations influencing the future of global healthcare. Tune in to watch the documentary segments airing in the second quarter of 2024 via the national airwaves, Bloomberg TV, and available on-demand via services like Amazon, Google Play Video, Roku, and several other channels.
Planet TV Studios is honored to host Gina Grad rejoining as the anchor. Gina excels as an acclaimed author, podcast moderator, and seasoned radio professional residing in Los Angeles, California. Previously, she worked as sharing the role of co-host and news anchor on the Adam Carolla Show, a celebrated podcast which broke the Guinness record for most downloads. Gina has been featured anchoring on KFI 640 AM as well as hosted the morning show on 100.3 FM. She presently presents "The Bryan and Gina Show, The Official Podcast of LA Magazine." Besides her on-air career, she has written "My Extra Mom," a storybook developed to aid kids and blended families in addressing the issues arising in blended familial situations.
Dr. Brandon Gough, M.D., is affirmed as a highly esteemed orthopedic surgeon, board-credentialed and acclaimed for his proficiency in hip and knee arthroplasty procedures across the community of Phoenix, Arizona. Employing state-of-the-art robotic technology alongside minimally invasive and muscle-preserving techniques, Dr. Gough endeavors to foster prompt returns to a rapid resumption of active living following surgery. His focus on maintaining soft tissue integrity not only expedites recovery but also minimizes hospital stays and, in some instances, permits patients to undergo total joint replacement procedures on an outpatient basis. He is known as a worldwide authority in the Direct Superior Approach complemented by muscle-sparing robotic techniques.
Dr. Gough views education as instrumental, enabling outstanding patient care through persistent engagement with orthopedic progress. After his initial studies at Spring Hill College situated in Mobile, Alabama, he embarked on his medical studies at Creighton University School of Medicine located in Omaha, Nebraska. He advanced his proficiency via residency and internship training in General Orthopedics at the University of Kansas, School of Medicine situated in Wichita, Kansas, where he gained the title of Resident Teacher of the Year. Further specialized training ensued during his fellowship in Lower Extremity Adult Reconstruction at the Arizona Institute of Bone and Joint Disorders.
Being board-certified by the American Board of Orthopedic Surgeons and actively involved with organizations like the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's steadfast commitment to excellence is evident beyond his medical practice. He serves as Vice President of the Orthopedic Surgery Interest Group and maintains memberships with the American Medical Association and American College of Physicians. He operates out of the renowned Orthopedic Institute of the West—which he helped establish—and has operating privileges at Scottsdale Abrazo Hospital, Liberty Hospital, along with select surgical centers in the Phoenix/Scottsdale, AZ area. With a fervent dedication to surgical innovation, he leads initiatives to create a center of excellence in robotic hip and knee replacement and concurrently disseminates his knowledge through training surgeons globally.
In parallel with his professional work, he ardently contributes to his community by volunteering with various charities including the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
Notably, Dr. Gough serves as a consultant and educator for Zimmer Biomet, further solidifying his commitment to advancing orthopedic care and surgical techniques.
Regarding Planet TV Studios: Planet TV Studios designs avant-garde, reality television series featuring comprehensive updates on critical business, medical, and socially impactful subjects.
Additional information on Gough Surgical, PLLC can be found at https://goughmd.com.
Additional series details are available at https://planettvstudios.com and https://planettvstudios.com/backstage/ or by contacting Christian Alain at 888-210-4292 x100 or at christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Steering Upcoming Era of Orthopedic Care
Inside the sphere of musculoskeletal surgery, precision, expertise, and novelty intersect at Gough Surgical Adult Hip & Knee, a celebrated establishment dedicated exclusively to adult lower joint replacements.
Under the masterful oversight of Dr. James Gough, this expert center has attracted accolades for elevating lifestyles by reinstating movement, reducing discomfort, and notably advancing well-being for many individuals.
Creating New Yardsticks in Orthopedic Interventions
Bone and joint surgeries, specifically related to hip and knee operations, form among the most frequently performed operations implemented worldwide.
Even so, the success statistics and patient experience ratings vary widely based on operative skill, facility quality, and the surgeon's methodology.
Gough Surgical stands apart by solely dedicating its practice to adult joint prosthetic surgeries, fostering concentrated know-how uncommon in the general field.
Dr. James Gough, renowned for his surgical precision and patient-centered care, has committed his professional life to perfecting these intricate operations.
His clinic, Gough Surgical Adult Hip & Knee, strategically located to cater to individuals from various areas, has become emblematic of high-quality results, quick recoveries, and high patient satisfaction metrics.
Superiority Based on Expertise
What motivates the exclusive specialization in adult hip and knee procedures?
Based on Dr. Gough's insights, dedicated specialization fosters unmatched competence.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," remarks Dr. Gough.
This specialized knowledge yields fewer complications, mitigated procedural risks, and improved patient experiences.
Progressive Operative Techniques and Technology
Gough Surgical Adult Hip & Knee consistently incorporates cutting-edge technology to augment operative precision and therapeutic outcomes.
One of the notable features of the clinic entails employing state-of-the-art robotic surgical systems.
These cutting-edge technologies afford surpassing accuracy, culminating in refined prosthetic placement personalized to the patient's anatomical needs.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," observes Dr. Gough.
Patient-Focused Care: Beyond a Simple Procedure
At Gough Surgical, the delivery of care extends past the surgical stage.
From initial assessment through complete post-surgery monitoring, customized, considerate care is maintained from start to finish.
This whole-person strategy secures physical recuperation and encourages emotional support and confidence throughout the treatment journey.
Dr. Gough reminds us, "Recognizing the distinct requirements, anxieties, and objectives of every patient is vital." Customized care markedly affects recuperation speeds and overall patient approval.
Thorough Pre- and Post-Operative Services
Gough Surgical’s pledge to complete patient management manifests through its detailed pre-surgical planning and meticulous post-surgery monitoring programs.
Tailored preoperative instruction classes, comprehensive patient workshops, and private consultation meetings fortify patients’ physical and mental states, lessening stress and supporting knowledgeable decision-making.
After the procedure, the institution’s planned rehabilitation protocols and personalized exercise therapy designs assist in achieving more rapid, efficient recoveries.
Individuals value the straightforward direction, consistent progress tracking, and convenient availability of expert counsel, significantly enhancing their rehabilitation experience.
State-of-the-Art Answers to Complex Problems
Gough Surgical Adult Hip & Knee is proficient in treating complicated cases that other facilities often struggle with.
From complex joint revisions to addressing severe arthritis conditions, this practice introduces pioneering treatments by means of advanced surgical methods, minimally invasive interventions, and individualized implant designs.
These specialized approaches often culminate in quicker recuperation, minimized post-surgery pain, and enhanced operational function, enabling a rapid resumption of dynamic, pain-free lifestyles.
A Heritage of Client Contentment
The testimonials from Gough Surgical’s patients speak volumes about the transformative impact of its care.
Clients regularly mention restored self-sufficiency, considerable alleviation of pain, and elevated overall life satisfaction after their surgeries.
"Walking without pain was something I never imagined possible again," affirms Mary Thompson, whose total knee replacement was performed at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," declares Mary Thompson subsequently.
Steady Research and Continued Learning
Beyond treatment excellence, Gough Surgical Adult Hip & Knee remains deeply involved in orthopedic innovation through persistent research and learning programs.
Dr. Gough frequently engages in clinical studies, offering critical insights that further orthopedic science and patient treatment methods.
Additionally, the center facilitates routine educational sessions and collaborative workshops, supporting professional growth among healthcare providers and progressively lifting industry norms.
An Innovative Perspective on Orthopedic Care
As the field of musculoskeletal treatment modernizes, Gough Surgical stays ahead of the curve, persistently incorporating novel technologies and techniques.
The practice’s vision of continuous improvement ensures patients receive the most advanced, effective treatments available.
"{Our goal is to redefine what's possible in orthopedic surgery continually," notes Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," continues Dr. Gough.
Closing Remarks: Charting New Paths in Hip & Knee Care
Gough Surgical Adult Hip & Knee stands prominent in orthopedic medicine by intertwining advanced operative strategies, specialized care, and nurturing patient engagement.
By relentlessly challenging the limits of current capabilities, Dr. James Gough and his committed staff not only restore joint functionality—they dramatically enhance lives.
In the quest for unhindered mobility and restored vigor, Gough Surgical Adult Hip & Knee is not just reshaping orthopedics—it is crafting the future benchmarks for medical care.
Micro-level & Muscle-Sparing Surgical Methods: Transforming Current Healthcare
In recent decades, surgical innovation has redefined health service delivery, delivering lower trauma, brisk healing, together with improved outcomes.
Among these advancements, micro-invasive and muscle-sparing surgical methods have materialized as revolutionary techniques.
These procedures have not only remodeled the operating environment, but also redefined the patient experience.
This article explores the evolution, techniques, benefits, challenges, and future directions of micro-invasive and muscle-sparing surgery, drawing on authoritative insights, scientific studies, and real-life applications.
A Novel Age in Surgical Practice: The check it out Climb of Minimally Invasive Procedures
Today’s surgical suite stands in stark contrast to the major incisions and lengthy inpatient stays that marked surgical procedures a century ago.
Surgical specialists today are more frequently employing procedures that lower tissue injury and conserve the inherent body structure.
Integral to these modernizations are found micro-invasive and tissue-sparing approaches.
This approach, micro-invasive surgery, implies techniques that use small incisions, specialized instruments, and high-definition imaging to access and treat internal conditions with minimal disruption to surrounding tissues.
Differently, tissue-sparing surgery centers on retaining muscle integrity in procedures that conventionally involved large-scale muscle cutting.
Both approaches belong to an expansive shift focused on diminishing patient complications, pain levels, and healing periods.
A Historical Review: Transitioning from Open Surgery to Tissue Preservation
Surgical practices have traditionally been influenced by necessity and the available technical means.
Preceding the era of modern imaging and state-of-the-art instrumentation, physicians had little choice but to execute large open incisions to ensure adequate exposure and reach the target site.
Even though these methods were life-preserving, they typically imposed substantial postoperative pain, extended recuperation, and increased the likelihood of complications like infections or persistent muscle debility.
The transition was marked by the introduction of laparoscopic surgery in the late 20th century—a minimally invasive procedure that permitted internal visualization by way of a tiny camera through small incisions.
With technological progress, surgeons increasingly recognized that safeguarding muscle integrity in procedures could yield superior advantages.
techniques for muscle preservation, first pioneered in orthopedics and cardiovascular surgery, rapidly extended to applications in abdominal, gynecological, and oncological procedures, along with others.
Dr. Eleanor Matthews , a trailblazer in minimally invasive surgical methods at a prominent teaching hospital, recounts: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This shift toward less invasive techniques stands as both a technical feat and a profound change in the approach to surgical care.
The Science Behind the Techniques
Micro-Invasive Procedures: Accuracy Empowered by Technology
At the core of micro-invasive surgery is the principle of precision.
Surgeons use an array of high-tech tools—from endoscopes and robotic-assisted devices to specialized microscopes—to navigate the human body through minuscule openings.
These tools yield improved magnification and light, which facilitates exact localization and treatment of the designated area without causing significant tissue harm.
One of the most significant innovations has been the integration of robotic-assisted surgical systems.
These systems enable an unprecedented level of stability and precision in surgery, filtering out hand tremors and translating slight movements into finely controlled actions.
In procedures such as prostatectomies and cardiac surgeries, this precision translates directly into improved patient outcomes.
Cardiothoracic Surgery: Minimizing Cardiac Trauma
Cardiothoracic interventions have notably advanced owing to micro-invasive techniques.
Procedures such as valve repairs and coronary artery bypass grafting (CABG) have traditionally required large incisions and extensive dissection of muscle tissue.
Nowadays, surgeons are steadily using minimally invasive approaches that rely on limited incisions and tailored instruments for accessing the heart and its surrounding anatomy.
Adopting robotic-assisted technology in cardiothoracic procedures has further elevated these methods.
In many cases, the robotic platform provides the precision required to perform delicate maneuvers on the beating heart, reducing the risk of complications and promoting faster recovery.
Research in the Annals of Thoracic Surgery established that patients receiving minimally invasive valve repairs experienced less postoperative atrial fibrillation and shorter hospitalizations compared to those undergoing conventional surgery.
General and Gynecologic Procedures: Improving Patient Results.
In general and gynecologic procedures, micro-invasive methods have markedly altered techniques such as cholecystectomies, hernia repairs, and hysterectomies.
This transition to limited incisions and muscle conservation not only diminishes visible scarring but also lessens postoperative pain and the likelihood of complications.
For example, the minimally invasive gallbladder removal procedure known as laparoscopic cholecystectomy has become the standard in many parts of the world.
Those undergoing the procedure enjoy shorter healing times and nearly immediate return find this to normal activities.
In gynecology, the implementation of muscle-preserving methods has led to improved outcomes for women undergoing complex procedures including myomectomies and pelvic floor repairs.
A leading medical journal’s review of clinical outcomes found that minimally invasive gynecologic surgeries lead to lower infection and blood loss rates, as well as superior cosmetic outcomes.
These benefits not only improve patient satisfaction but also translate into enhanced overall health outcomes.
Weighing the Benefits and Challenges.
Outcomes That Extend Outside the Operating Room.
The advantages of micro-invasive and muscle-sparing surgical methods extend well beyond the technical aspects of surgery.
For patients, the benefits are tangible and life-changing.
Lower pain levels, decreased scarring, and quicker recovery periods directly contribute to a higher quality of life.
In many cases, patients can return to work and resume daily activities within days rather than weeks, a critical factor in an increasingly fast-paced world.
On a broader scale, these approaches lower hospital costs by reducing both the duration view publisher site of inpatient care and the necessity for extensive postoperative support.
Additionally, lower complication rates lead to fewer readmissions, a crucial benefit for both healthcare providers and insurers.
The psychological advantages are important and must not be underestimated.
Knowing that a procedure can be performed with minimal impact on one’s body provides reassurance and reduces preoperative anxiety.
This point is especially important for major surgical cases, where a positive and calm mindset contributes to improved overall outcomes.
Challenges and Limitations: A Realistic Perspective.
Even with their many benefits, minimally invasive and muscle-preserving methods come with their own set of challenges.
One significant limitation is the steep learning curve associated with these advanced methods.
Surgeons must undergo rigorous training and gain substantial experience before they can perform these procedures with the same level of proficiency as traditional surgeries.
The high cost of advanced equipment and intensive training can reduce accessibility in under-resourced settings.
Furthermore, patient suitability varies and not all are ideal candidates for these methods.
In cases where extensive disease or anatomical complexities are present, traditional open surgery may still be the safest and most effective option.
Surgeons must carefully assess each case, balancing the potential benefits of minimally invasive techniques against the specific needs of the patient.
Technical challenges also factor into the overall limitations.
Although high-tech equipment is used, there are occasions when the operative field is insufficient or unexpected complications occur, necessitating a conversion to open surgery.
These scenarios, while relatively rare, highlight the importance of having a versatile surgical team that is prepared to adapt to changing circumstances.
Authority Insights and Patient Testimonials
Echoes from the Frontline
Dr. Michael Andersen, a renowned surgeon with 25+ years of experience in minimally invasive procedures, asserts the importance of personalized care
“Every patient is unique, and while micro-invasive and muscle-sparing techniques offer tremendous benefits, the key is to tailor the approach to the patient’s specific condition and overall health,” he states.
His understandings underscore a vital tenet of modern medical practice: that technology must be subservient to the patient’s needs, not prescriptive in treatment.
In the same way, patients who have experienced these procedures often talk about the remarkable, life-altering impact they have encountered.
Maria Lopez, a 54-year-old woman who recently underwent a muscle-sparing breast reconstruction, describes her journey.
“I anticipated a lengthy and challenging recovery, yet to my surprise, I was up and moving in mere days. It truly felt like a new beginning in life,” she remarks.
Though anecdotal, these accounts are bolstered by robust clinical evidence demonstrating improved outcomes with these procedures.
Building a Trustworthy Surgical Ecosystem.
The growing popularity of micro-invasive and muscle-sparing methods is fostering a broader cultural shift in healthcare.
Surgeons, hospitals, and training programs are increasingly collaborating to share best practices, develop standardized protocols, and invest in ongoing research.
Scheduled conferences and symposia on minimally invasive techniques have become regular fixtures in medicine, offering forums for experts to explore innovations, challenges, and future directions.
This collaborative approach is essential for addressing the challenges associated with these advanced techniques.
By pooling expertise and resources, the medical community is better positioned to refine surgical methods, reduce complications, and ensure that the benefits of these techniques are accessible to a wider population.
The Future of Surgery: Trends and Innovations.
Integrating Artificial Intelligence and Robotic Technologies.
While current micro-invasive and muscle-sparing techniques have already made a profound impact, the future promises even more dramatic changes.
The merging of AI and machine learning with surgical systems is anticipated to elevate precision and operational efficiency even further.
These technologies can analyze vast amounts of data in real time, offering surgeons predictive insights that may improve decision-making during complex procedures.
For instance, AI-powered imaging solutions are being developed to automatically underscore essential anatomical structures, thereby diminishing the risk of accidental injury.
Robotic systems are rapidly advancing, with next-generation platforms offering exceptional control and enriched haptic feedback that lets surgeons “feel” the tissue they work on—a trait missing from conventional laparoscopic equipment.
Extending the Frontiers of Minimally Invasive Procedures.
Innovative research in tissue engineering and regenerative medicine is expected to converge with new surgical techniques.
Scientists are exploring ways to not only minimize tissue damage but also promote faster, more natural healing.
This includes the use of bioengineered scaffolds that can support tissue regeneration and reduce scar formation after surgery.
Moreover, as imaging and sensor technology continue to improve, surgeons may be able to perform procedures that are even less invasive than those currently available.
Technologies such as nanorobots and small, implantable devices may eventually provide targeted therapy and diagnostics on a cellular scale, paving the way for truly customized medicine.
An International Standpoint: Narrowing the Divide in Surgical Services
Although groundbreaking technological advancements are redefining surgery in developed nations, substantial imbalances in access to modern surgical care remain globally
Bridging this gap calls for unified efforts from governmental bodies, non-profit entities, and the worldwide healthcare sector
Training initiatives, technology exchange projects, and collaborative research ventures are crucial for ensuring that individuals worldwide benefit from innovations in minimally invasive and muscle-preserving surgery
Global alliances are already revealing encouraging prospects
Institutions in high-resource regions are working in tandem with hospitals in developing locales to provide training and support for minimally invasive surgical techniques
Such partnerships improve patient outcomes while simultaneously fostering a more equitable and robust global healthcare system
Mapping the Future Course: Hurdles and Promising Prospects
The advancement toward full-scale integration of minimally invasive and muscle-sparing techniques is accompanied by various obstacles
The capital investment required for high-end surgical equipment, along with the necessity for specialized instruction, is considerable
Still, the lasting improvements in treatment outcomes and healthcare cost efficiencies demonstrate that these difficulties are manageable
Healthcare decision-makers are increasingly aware that investing in innovative surgical methods can deliver impressive returns
Abbreviated hospitalizations, reduced complication rates, and an expedited return to normal activities not only enhance patient well-being but also support a more effective and enduring healthcare structure
As a result, both public and private stakeholders are directing greater resources toward the evolution and propagation of these advanced techniques
Additionally, there is a transformative shift occurring within the surgical profession's culture
A prioritization of enduring learning, joint multidisciplinary engagement, and rigorously tested practices is crafting a climate where innovation is simultaneously supported and demanded.
This metamorphosis in cultural approach is expected to streamline the incorporation of new techniques and advanced technological tools, ultimately favoring better patient outcomes.
Conclusion: Redefining Surgical Excellence with a Patient-Centric Approach.
The advancement of micro-invasive and muscle-preserving techniques marks a revolutionary turning point in how surgical care is administered.
These methods have reshaped operative protocols by emphasizing precision, limiting invasive trauma, and maintaining muscle function, thereby boosting clinical outcomes and patient experience.
From the early innovations in laparoscopy to the contemporary synergy of robotics and AI, the progression exemplifies relentless innovation and a persistent pursuit of excellence.
For patients, these methods promise less postoperative pain, faster recuperation, and an improved overall quality of life.
For surgical teams and healthcare experts, the challenge is mastering these innovative approaches, investing in breakthrough technologies, and sustaining a culture of continual enhancement.
With the steady march of scientific research and technology, the potential for new innovations in these surgical techniques remains impressive.
The future of surgery envisions a patient-centric model where the well-being of the individual is paramount and surgical tools are designed to augment, not undermine, the body’s inherent resilience.
Looking ahead, the convergence of advanced imaging, robotics, and regenerative medicine is set to unlock unprecedented frontiers in patient-centered care.
The ever-progressing landscape of surgical practices is a tribute to the healthcare community’s enduring commitment to innovation, safety, and enhanced patient outcomes.
As individualized healthcare becomes the norm, micro-invasive and muscle-sparing techniques emerge as symbols of a future where interventions are less traumatic and patient outcomes are significantly improved.
The journey goes on, and each breakthrough takes us closer to transforming surgery from a harbinger of pain and prolonged convalescence into a gateway to revitalized health and energy.
Source Materials and Additional References.
Clinical Studies and Reviews: Various clinical studies in esteemed journals including the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education deliver compelling data on patient results and the advantages of these approaches.
Expert Interviews: In-depth conversations with leading surgeons—such as Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen—provide invaluable insights into the practical applications and challenges of adopting micro-invasive and muscle-sparing techniques.
Technological Innovations: The evolution of robotic-assisted surgical techniques and the integration of augmented reality are captured in modern literature and widely discussed at global surgical events.
The advent of micro-invasive and muscle-preserving surgery has redefined patient-centered care by prioritizing precision, reducing surgical trauma, and maintaining muscle function to improve both clinical outcomes and patient quality of life.
As innovation in technology accelerates and healthcare providers worldwide adopt these breakthroughs, the future of surgery promises even more significant advantages for patient care.
In this rapidly advancing field, the steadfast commitment to continuous improvement remains the true measure of progress—a promise that will ultimately redefine surgical care for generations to come.
 Alfonso Ribeiro Then & Now!
Alfonso Ribeiro Then & Now!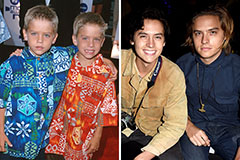 Dylan and Cole Sprouse Then & Now!
Dylan and Cole Sprouse Then & Now!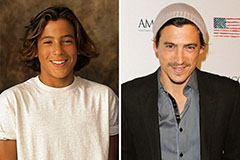 Andrew Keegan Then & Now!
Andrew Keegan Then & Now! Tina Majorino Then & Now!
Tina Majorino Then & Now!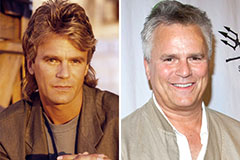 Richard Dean Anderson Then & Now!
Richard Dean Anderson Then & Now!